This is a monthly update on my glycemic management of type 1 diabetes (T1DM) using Humalog and Lantus insulin injections with resistance exercise and a ketogenic real-food diet as described in my book, The Ketogenic Diet for Type 1 Diabetes also available on Amazon in print. My coauthor, Ellen Davis, over at the Ketogenic-Diet-Resource.com website and her team have come out with a new ketogenic meal planning tool. It’s called KetoPoints and it uses a points-based system to make ketogenic meal planning really easy. The app includes starter meals, five informative guides on getting started and staying on track, a step-by-step process for building each meal, cooking directions and more. In addition, new, personalized meals will be added to the program monthly. You can sign up for a 3 week challenge or go for a monthly subscription. I have not used the tool myself, but it may be helpful for those just getting started with a ketogenic diet.
I had stopped eating sweet potato (on August 24) to understand if the extra carbohydrate had a positive effect on my strength. On September 17, I set two personal bests in my weightlifting: a 165 lb. snatch and 215 lb. clean & jerk which occurred 6 months after my previous personal best of 209 lb. on March 26, 2017. During the remainder of September, my weightlifting results were better than when I was taking sweet potato. Thus, I feel that the extra 30 grams of carbohydrate was not helping my performance. In September, continued once daily weightlifting workouts with only two exercises per day lasting about 2 hours including warmup, rest between lifts, and cool down.
Glycemic Management Results for September 2017
My September glycemic results were noteworthy for low BG readings requiring a reduction in insulin doses during the month. Fortunately, I had no symptoms of hypoglycemia in September. Hypoglycemia in a person with T1DM who is conscientiously trying to control BG is a real danger that should be minimized. However in September, I had much more hypoglycemia than usual.
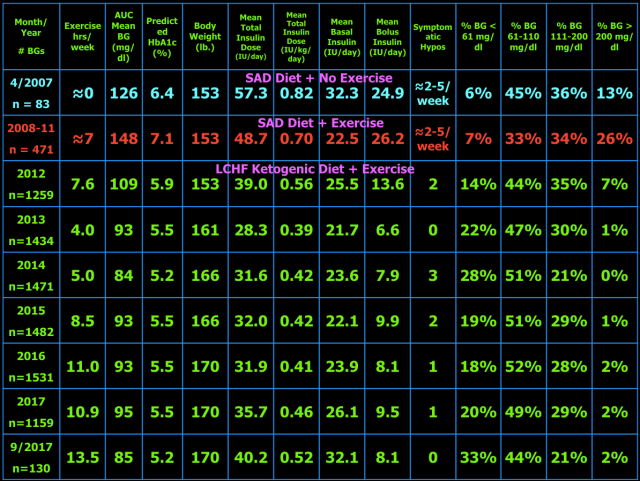
Below are my mean BG values, mean insulin doses, and BG frequency distribution for September 2017 compared to previous time periods. I have changed two columns to indicate the AUC mean BG and predicted HbA1c. AUC mean BG is the mean BG by calculating the area under the curve (AUC) of BG versus time. The predicted HbA1c uses the formula: AUC mean BG plus 88.55 divided 33.298. This formula is the least squares fit using my own personal mean BG versus measured HbA1c over many years. My particular HbA1c values are higher than many other individuals with the same mean BG. This is referred to as being a “high glycator.”
As presented in blog post #15 exogenous insulin cannot mimic normal insulin secretion, so persons with T1DM should not expect to have truly normal BG values at all times. They just need to be low enough to prevent long-term complications and not so low as to cause unpleasant hypoglycemic symptoms or less common but dangerous consequences including brain damage, seizure, injury, coma, or death. I have set my target BG range at 61-110 mg/dl because values in this range are not likely to lead to harm or complications of T1DM. Your target BG range should be determined with your physician because one size does not fit all. Normal BG is 96 ± 12 mg/dl (mean ± standard deviation (SD)) and coefficient of variation is 13% which is the weighted mean from these two studies (here and here) of continuous glucose monitoring in healthy subjects. The standard deviation and coefficient of variation are measures of BG variability which I believe are important in T1DM. However, be advised that clinical outcomes in T1DM (i.e. microvascular and macrovascular complications) have only been documented to correlate with measures of mean BG, particularly HbA1c. This does not mean that BG variability is not important, but it just has not been documented to correlate with outcomes and complications of T1DM. Achieving a normal standard deviation or coefficient of variation in T1DM would be difficult, if not impossible, with current exogenous insulin therapy (injected or pumped). Monitoring the standard deviation and/or coefficient of variation and finding ways to improve them to the best of one’s ability is desirable in my opinion. Following a low carbohydrate ketogenic diet is one such method of reducing BG variability, mean BG, insulin doses, and hypoglycemia. A ketogenic diet may also provide an alternate/additional brain fuel in the form of ketones to protect the brain when BG does go low. The alternative energy that ketones supply to the brain may prevent or blunt the sympathoadrenal response to hypoglycemia which in turn reduces or eliminates the symptoms of and harm from hypoglycemia. This hypothesis needs to be tested before it can be stated as fact. Having BG close to normal most of the time (some of which are hypoglycemic) also minimizes the symptoms of mild hypoglycemia and potentially the harm from hypoglycemia as well due to lack of activation of the sympathetic nervous system and adrenal gland responses to hypoglycemia i.e. sympathoadrenal-induced fatal cardiac arrhythmia, see here.
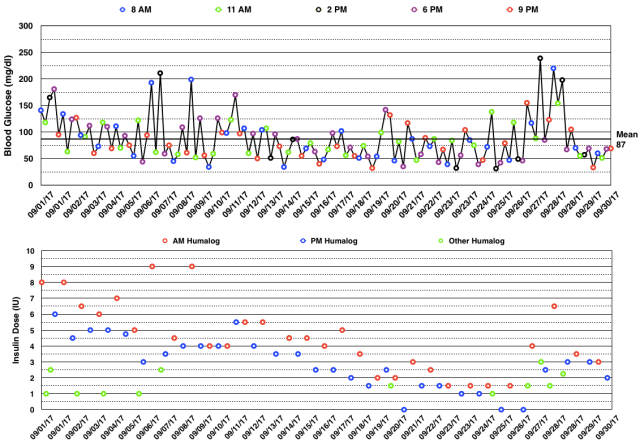
Below are my BG readings along with the Humalog (rapid-acting insulin) doses in September 2017. You can see below that both the morning and evening meal-time doses had to be decreased due to low BG readings. Many of these low BG readings occurred during/after weightlifting which previously resulted in hyperglycemia. The point here is that a basal insulin dose that is higher than current needs can override any stress hormone response to intense resistance exercise. Those without diabetes can experience an increase in BG with intense exercise, see here.
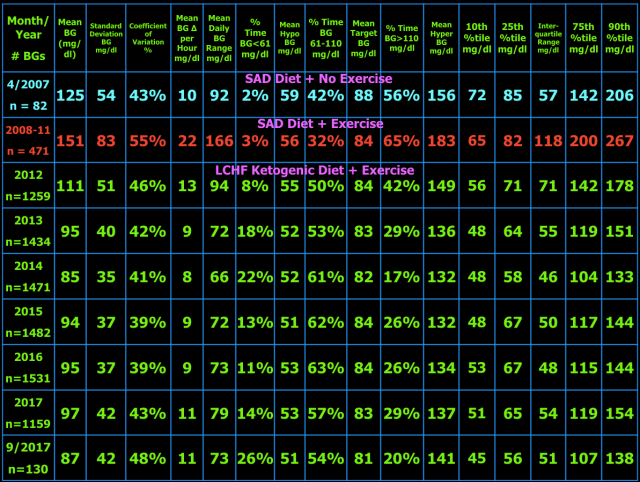
The table below shows the BG variability results for current and previous time periods. The percentiles (10th, 25th, 75th, 90th) on the right show the spread of the BG readings about the median. The interquartile range, the difference between the 75th and 25th percentiles, is a measure of BG variability. In the middle of the table are the %Time in three BG ranges: %Time BG < 61 mg/dl (hypo) and the mean BG during that time, then %Time BG 61-110 mg/dl (target) and the mean BG during that time, and %Time BG > 110 mg/dl (hyper) and the mean BG during that time. The other measures of BG variability were defined and explained in blog post #10.
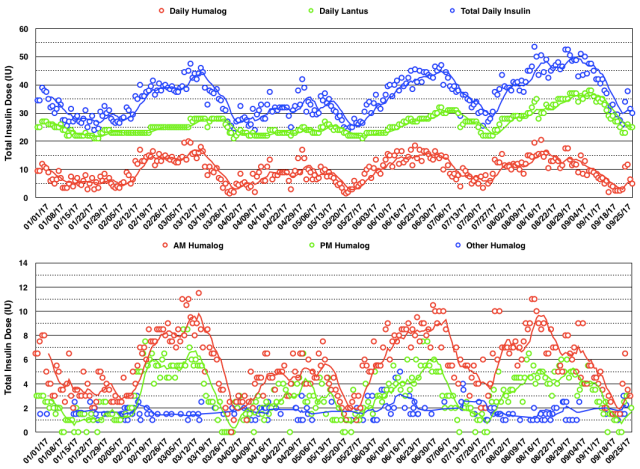
The daily insulin dose totals and BG readings are shown in the graphs below. You can see that I had to decrease my total insulin dose progressively during the month from 53 IU/day to 30 IU/day.
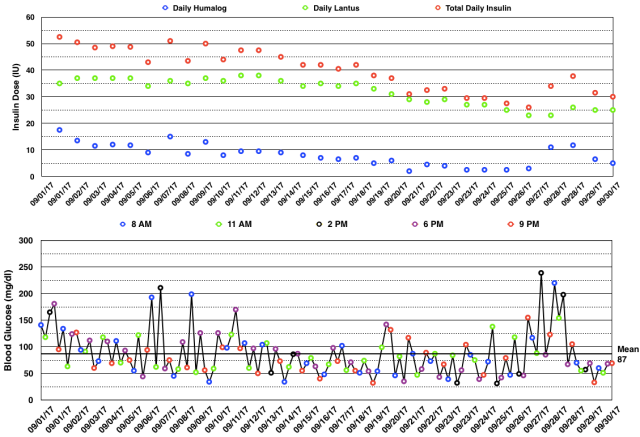
The daily insulin dose totals for 2017 are shown in the graph below. You can see an oscillatory pattern with a period of about 8 weeks. The cause for this is unclear at this point, but I am making changes in my insulin dosing procedures and will followup on this next month.
In October, I will continue olympic weightlifting every day with just two exercises per day.
My Thoughts About Management of Type 1 Diabetes With A Ketogenic Diet
My goal of glycemic management in T1DM with a ketogenic diet is to keep BG as close to normal i.e. 96 ± 12 mg/dl (mean ± SD) as is safely possible (i.e. avoiding hypoglycemia) to avoid diabetic complications, a reduction in lifespan, and unpleasant symptoms of as well as injury and death from hypoglycemia. For me, a well-formulated whole-food nutrient-dense ketogenic diet, daily exercise, frequent BG measurements, and lower insulin-analog doses (Humalog/Lantus) have improved my glycemic control, hypoglycemic reactions, and quality of life. My current version of ketogenic diet has changed slightly since I last wrote about it in detail in blog post #9.
My current diet looks like this.
What I Cook & Eat
- Beef, grass-fed, including meat (85% lean), heart, liver, and kidney (liverwurst)
- Fish, mainly wild Alaskan salmon
- Canadian bacon (uncured pork loin)
- Lamb occasionally
- Chicken & Turkey occasionally
- Chicken Eggs
- Non-starchy vegetables (about 5% carbohydrate content by weight) including Cabbage (Red, Green, Napa), Kale, Collard Greens, Spinach, Bell Peppers, Leeks, Onions, Brussels sprouts, Home-made Sauerkraut from Red Cabbage, Bok-Choy, Broccoli, Cauliflower, Yellow Squash, Zucchini, Cucumber, Lettuce (Iceberg & Romaine), and some others.
- Fruit – Avocado, Tomatoes, Olives, Strawberries, Blueberries, Blackberries, lemon juice on fish and salads
- Root Vegetable: Raw Carrots
- Nuts & Seeds – Pepitas, Macadamia, Brazil, Pecan, Walnut, Pistachio, Cashew.
- MCT oil – a few tablespoons on salads
- Note: I developed an intolerance to milk prior to my diagnosis of T1D. I did try heavy whipping cream after starting my KLCHF diet, but am also intolerant of it. I do tolerate butter, but wanted to decrease my fat intake, so eliminated all dairy including cheese and yogurt.
What I Drink
Water (filtered by reverse osmosis), Unsweetened Tea & Coffee
What I Don’t Eat
- Grains – Wheat, Corn, Rice, Oats (there are many more) or anything made from them, which is too numerous to list here. Gluten is a protein present in a number of grains (all varieties of wheat including spelt, kamut, and triticale as well as barley and rye.) which can cause a number of medical problems for a significant portion of the population with gluten sensitivity or celiac disease. In my case, I avoid them due to their carbohydrate content.
- Starchy and most root vegetables – potatoes, sweet potatoes, yams
- Legumes – peas, beans, lentils, peanuts, soybeans
- High sugar fruits – includes most fruits except berries, see above.
- Sugar and the fifty other names used to disguise sugar.
- Vegetable Oils – Canola, Corn, Soybean, Peanut, Sunflower, Safflower, Cottonseed, Grape seed, Margarine & Butter substitutes, Shortening.
- All Processed Food-like Substances i.e., most of what is in the grocery store.
- I avoid restaurants except when traveling, and then order fish or steak with plain steamed non-starchy vegetables (no gravy or sauces that typically contain sugar, cornstarch, or flour) or salad.
- Refined, but healthy, fats – I have eliminated refined fats except MCT oil from my diet including butter, coconut & olive oils to improve body composition and remain in the 77kg olympic weightlifting weight class.
What I Don’t Drink
- Colas (both sweetened, artificially sweetened, and unsweetened).
- Fruit Juice except small amounts of lemon juice.
- Alcohol (can cause hyperglycemia or hypoglycemia in persons with diabetes).
- No artificial sweeteners, don’t need or like them.
When my entire diet is analyzed, 26% of my fat intake is from polyunsaturates (mainly from nuts and seeds), 56% is from monounsaturates, and 18% is from saturated fats. When my diet is broken down by macronutrients, I consume 170 grams of fat (or 68% of my total daily calories), 70 grams of carbohydrate, 30 grams of which is dietary fiber (or 12% of my total daily calories), and 110 grams of protein (or 20% of my total daily calories). In calories, it totals to 2,250 kcal/day.
My exercise regimen makes glycemic management more challenging, but I enjoy exercise and feel it has other health and lifespan-extending benefits. Hopefully, my BG values and variability as well as my lower insulin doses that result from my ketogenic diet and exercise are close enough to optimal to avoid any reduction in lifespan, diabetic complications, and harm from hypoglycemia, but only time will tell.

Hi Keith,
We also use Lantus, but recently I came across in Dr. Bernstein’s book (p. 286) that he does not use or recommend Lantus. Have you tried a different long lasting insulin and what is your opinion about it? Thank you,
Svet
LikeLike
Hi Svet. Dr. Bernstein does not recommend Lantus because some early association studies found an increased relative risk of cancer in those with type 2 diabetes using Lantus. Persons with type 2 diabetes have an increased risk of cancer due to their insulin resistance which is not usually present in type 1 diabetes, especially in normal weight children with type 1 diabetes. Subsequent studies could not confirm that association and the issue of Lantus and cancer was deemed to be a non-issue. I don’t know if Dr. Bernstein is aware of the more recent studies. Either way, association studies can never prove cause and effect, only association or correlation. That means they cannot prove that Lantus causes cancer.
I did try Levemir after reading Dr. Bernstein’s book, but it did not work for me as well as Lantus. Currently, he has changed from recommending Levemir and is recommending Tresiba (insulin degludec) which is an ultralong-acting basal insulin analogue. It may have advantages for some who feel that Lantus or their current long-acting insulin is not lasting a full 24 hours, but undoubtedly would come at a greater financial cost. I’m sticking with Lantus for now.
LikeLiked by 2 people
Thank you! I was not aware that the study was referring to type 2 diabetes. It made me a bit concerned because Lantus seems to work for us for now.
LikeLike
Here is one of the studies from Germany. They searched pharmacy records for a diagnosis of diabetes mellitus. They were unable to distinguish type 1 or 2, but since the majority of people taking insulin are type 2, this association study would apply primarily to type 2. Here is another similar study from Scotland. They did not find an association of Lantus with cancer. This is a commentary on the topic titled Glargine and Cancer: Can We Now Suggest Closure? which explains what I said in more detail. I personally am not worrying about getting cancer from taking Lantus.
LikeLiked by 1 person
Hey Keith – Do you have an opinion on Dr. Bernstein’s claim that 83 mg/dL is normal blood sugar? I notice that on all your posts, you have a section at the bottom discussing how you aim from 96 +/-12 mg/dL. I’m curios because I find that 96 is a much easier target to hit. I really trust Dr. B, but I’m wondering if I should adjust my targets to be more like yours. I must admit that I physically feel a lot better when I wake in the morning with a 96 than I do if I wake with a 76 (though I get happier with the 76 because I feel like it’s better for my A1c). So, what do you think about Dr. B’s 83mg/dL?
LikeLike
Hi Brian, I aimed for Dr. Bernstein’s 83 mg/dl when I started my low carb diet based on his book. The story he tells about how he arrived at that number was that was the reading that home glucose monitor representatives who visited his office had when Dr. Bernstein asked them to demonstrate their meter to him. This did not take into account any rises in blood glucose (BG) after meals which would be normal. In 2014 I achieved an average BG of 85 mg/dl, but 22% of the time I had a BG of less than 61 mg/dl which I did not think was good. So I decides to research what really is the BG in normal people without any signs of insulin resistance. I found only two studies that monitored glucose during a 24 hour day using both BG and interstitial continuous glucose monitors. Normal BG is 96 ± 12 mg/dl (mean ± standard deviation (SD)) and coefficient of variation is 13% which is the weighted mean from these two studies (here and here) of continuous glucose monitoring in healthy subjects. Thus, I changed my target to 95 mg/dl and had a reduction in time spent with hypoglycemia ever since. Hope that helps you.
LikeLiked by 1 person
Hello, Keith.
I’ve had been able to buy your book (Amazon). Thank you for the advice, because I have found information about diabetes I had never been told from my doctors and also lots of academic references.
I just have one doubt, as we can read in your book we shouldn’t fear eating fat. My daily caloric intake is between 3500 and 4500 kcal, depending on the intensity of the exercise. Between 6% and 7% of calories comes from carbohydrates (between 50g and 70g), and between 77% and 80% come from fat (almost 500g!). In your opinion, is not that too much fat? My weight is stable, but if I eat less, I have noticed that I lose weight. My ketones are 0,7 mmol.
Thank you.
LikeLike
Hi Eric. I assume you are a large person who is very physically active from the daily caloric range you have mentioned. If you are lean with a body fat percentage in the range of 8-20% and your protein intake is in the range of 1.0-1.5 grams/kg body weight/day and that results in eating almost 500 grams of fat from the healthy food sources listed in the book, then I would say that is just fine. Your blood ketone level is fine, higher is not necessarily better. Dietary fat only becomes a problem when it is accompanied by a diet containing a lot of refined carbohydrates and/or sugars and/or there is an excess caloric intake that results in excess body fat. As an aside, 500 grams of fat is 4500 calories, so I suspect your actual fat intake is significantly less assuming your total daily caloric intake is between 3500 and 4500 kcal per day.
LikeLike
Thank you for the answer.
Yes, sorry for the number: I meant “almost 400g!”. Always healthy fat and from the options you recommend in the book. The daily range would be 300g-400g, depending on the exercise. When I do a longer aerobic exercise (from 4h to 5h ride) my fat intake increases until 400g (I eat avocado, cheese and nuts, and my BG is always stable).
I am in fact in the second group, quite lean: 135 pounds (5 ft and 8.5 inches). The problem is that I am over your recommendation of protein intake (2.0-2.5 grams/day), but I fear reducing protein because then I would have to increase my fat intake, which I already thought was high. Furthermore, when doing sports, in addition to fat I eat more protein (because of cheese and nuts…). I think I am doing something wrong, there. In your opinion, should I try to decrease protein intake, then?
Thank you again.
LikeLike
A protein intake of 1.0-1.5 grams/kg body weight/day covers most, but not all, people. Nutrition should be individualized and one size does not fit all. Athletes in general should be taking more protein, but the exact amount is not really known. If you feel and perform well with your current diet, I would not change it.
LikeLike