Whereas February 2017 was my best one month glycemic control to date, March was rather typical of the previous two years or so. This was in part due to changing insulin doses, both increases and decreases, which continue for reasons not altogether clear to me since I am just responding to and correcting high and low blood glucose (BG) readings. Another factor in BG fluctuations in March was travel for a week that was also highlighted with a symptomatic hypoglycemic episode: the first one in 2017. Travel has always resulted in more hypoglycemia and hyperglycemia due to changes in diet, exercise, sleep patterns, time zones, and possibly stress. During my trip I also participated in my second olympic weightlifting meet on March 26th in San Diego, CA where I lifted 72 kg in the snatch and 95 kg in the clean & jerk for a total of 167 kg, an 8 kg improvement compared to my first meet total of 159 kg. I made 5 of 6 lifts to achieve that total. The hypoglycemic episode mentioned above occurred after dinner on the day of the weightlifting meet.
Glycemic Management Results for March 2017
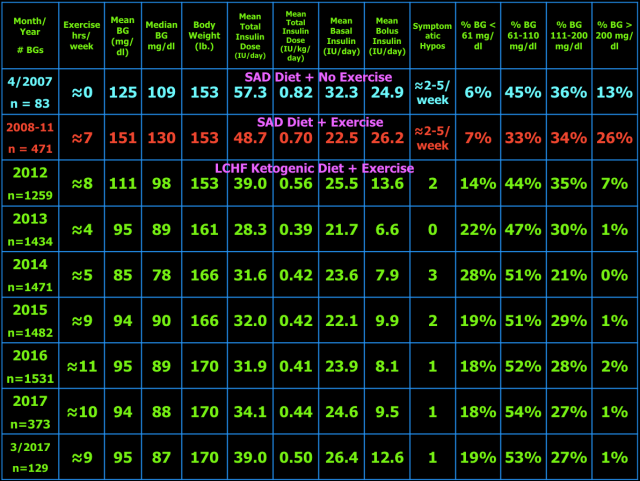
Below are my mean blood glucose (BG) values, insulin doses, and BG frequency distribution for March 2017 compared to previous time periods.
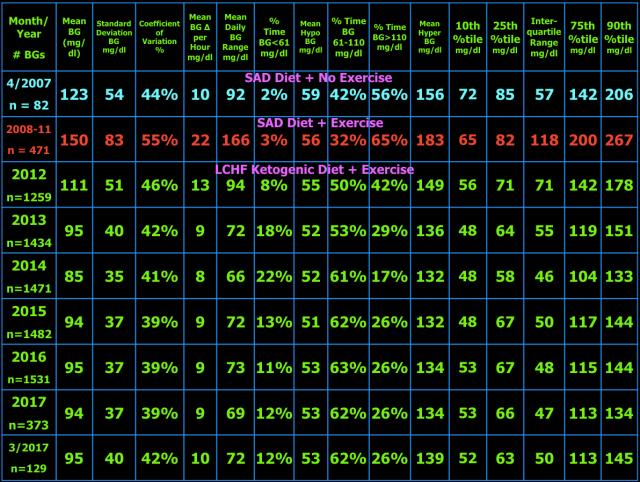
As presented in blog post #15 exogenous insulin cannot mimic normal insulin secretion, so persons with type 1 diabetes (T1DM) should not expect to have truly normal BG values. They just need to be low enough to prevent long-term complications and not so low as to cause unpleasant hypoglycemic symptoms, brain damage, seizure, injury, coma, or death. I have set my target BG range at 61-110 mg/dl because values in this range are not likely to lead to harm or complications of T1DM. Your target BG range should be determined with your physician because one size does not fit all. Normal BG is 96 ± 12 mg/dl (mean ± standard deviation (SD)) and coefficient of variation is 13% which is the weighted mean from these two studies (here and here) of continuous glucose monitoring in healthy subjects. The standard deviation and coefficient of variation are measures of BG variability which I believe are important in T1DM. However, be advised that clinical outcomes in type 1 diabetes (i.e. microvascular and macrovascular complications) have only been documented to correlate with measures of mean BG, particularly HbA1c. This does not mean BG variability is not important, but just that measuring BG variability over long periods of time in numerous individuals with T1DM is more difficult so very few trials have attempted to measure it. Achieving a normal standard deviation or coefficient of variation in T1DM would be difficult, if not impossible, with current exogenous insulin therapy. I hope that adding a continuous glucose monitor (CGM) to my therapeutic regimen will improve my BG control. I plan to get the FreeStyle Libre CGM as soon as it becomes available in the U.S. Monitoring the standard deviation and/or coefficient of variation and finding ways to improve them to the best of one’s ability is desirable in my opinion. Following a low carbohydrate ketogenic diet is one such method of reducing BG variability, mean BG, insulin doses, and hypoglycemia. The ketogenic diet may also provide an alternate/additional brain fuel in the form of ketones to protect the brain when BG does go low. The alternative energy that ketones supply to the brain may prevent or blunt the sympathoadrenal response to hypoglycemia which in turn reduces or eliminates the symptoms of and harm from hypoglycemia. This hypothesis needs to be tested before it can be stated as fact. Having BG close to normal most of the time also minimizes symptoms of mild hypoglycemia and potentially the harm from hypoglycemia as well due to lack of activation of the sympathetic nervous system and adrenal gland responses to hypoglycemia i.e. sympathoadrenal-induced fatal cardiac arrhythmia, see here.
Below are my BG readings along with exercise type and time for March 2017.
The table below shows the BG variability results for current and previous time periods. The percentiles (10th, 25th, 75th, 90th) on the right show the spread of the BG readings about the median. The interquartile range, the difference between the 75th and 25th percentiles, is a measure of BG variability. In the middle of the table are the %Time in three BG ranges: %Time BG < 61 mg/dl and the mean BG during that time, then %Time BG 61-110 mg/dl, and %Time BG > 110 mg/dl and the mean BG during that time. The other measures of BG variability were defined and explained in blog post #10.
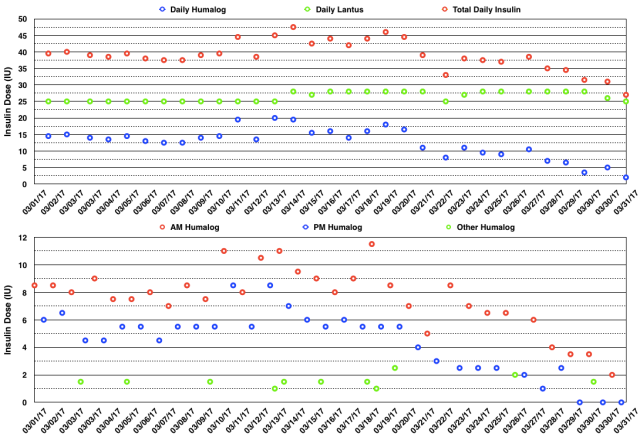
The actual daily insulin doses and daily insulin dose totals are shown in the graphs below. I had to take multiple extra rapid-acting insulin doses to correct hyperglycemia and the breakfast and dinner rapid-acting insulin doses increased in the second half of the month. I made small changes in my basal insulin doses based on the fasting BG results as usual. I still find it interesting that my insulin doses vary so much over time for reasons that I largely do not understand. Again, this is IMO due to the very nature of exogenous insulin therapy.

I am omitting my Ketonix breath acetone results this month since I did not take many measurements in March.
In April, I will continue olympic weightlifting most days by adjusting the load (intensity times repetitions) to avoid injury and overtraining and do aerobic exercise (swimming, rowing, or cycling at low intensity for ≈ 0.5 – 2 hours) the remainder of the days.
My Thoughts About Management of Type 1 Diabetes With A Ketogenic Diet
My goal of glycemic management in T1DM with a ketogenic diet is to keep BG as close to normal i.e. 96 ± 12 mg/dl (mean ± SD) as is safely possible (i.e. avoiding hypoglycemia) to avoid diabetic complications, a reduction in lifespan, and unpleasant symptoms of as well as injury and death from hypoglycemia. For me, a well-formulated whole-food nutrient-dense ketogenic diet (see blog post #9 for more details), daily exercise, frequent BG measurements, and lower insulin-analog doses (Humalog/Lantus) have improved my glycemic control, hypoglycemic reactions, and quality of life. I also feel, but cannot prove, that this eating plan and the resulting nutritional ketosis reduces the symptoms of hypoglycemia and protects the brain from the consequences of moderate degrees of hypoglycemia (see blog post #12 for more details). I also think that hypoglycemia unawareness (due to my frequent asymptomatic hypoglycemic episodes) contributes to my lack of symptoms of hypoglycemia. As pointed out in blog post #29, this may not necessarily be a bad thing. Exercise with its resulting varying insulin sensitivity and hormonal changes actually makes glycemic management more difficult i.e. challenging, but I enjoy exercise and feel it has other health and lifespan-extending benefits. Hopefully, my BG values and variability as well as my insulin doses are close enough to optimal to avoid any reduction in lifespan, diabetic complications, and harm from hypoglycemia. Only time will tell.
Till next time ….

Regarding your after dinner hypo : at what time did you do the weightlifting, at what time did you have dinner, and at what time did you have the hypo ? I’m just trying to gather info on muscle resistance exercises and hypo timings. I’m T1 and about to add weights & resistance to cardio. Thanks in advance.
LikeLike
The weightlifting meet started at 11 am and I finished about 12:30 pm on 3/26/2017. Since my body weight is a few kilos below my weight class (77 kg), I decided to eat breakfast prior to weigh-in at 9 am. My fasting blood glucose (BG) was 141 mg/dl so I took 6.5 IU Humalog breakfast bolus. After the Humalog had finished working 2.5 hrs after the dose at 9:30 am, BG was 123 mg/dl. After my lifts were finished my BG was 184 mg/dl which is not unusual (stress hormones are increased by intense exercise). I took a 2 IU Humalog correction dose and 2.5 hours later, my BG was 108 mg/dl. Prior to dinner (at 6:30 pm) my BG was 61 mg/dl and I took a smaller than usual Humalog dose of 2 IU with dinner along with 28 IU of Lantus. Two hours later, I was not not behaving normally (laughing for no particular reason) and was sweating and my BG was LO on my Freedom Freestyle meter which means <20 mg/dl (That is the lowest I have ever recorded and were I not on a ketogenic diet probably would have had a seizure or worse). It took a total of 6 glucose tablets (24 grams of dextrose, also a first, usually I take 1-2 tabs for a hypo) to bring it up to 75 mg/dl. I gave you these details because you asked. However, the BG response to exercise is quite variable and not predictable unfortunately. My BG has dropped during weightlifting and has also remained unchanged. Seems the determining factor is the intensity of the exercise and the basal dose of insulin (Lantus) at the time. My suggestion is to be prepared for both increases and decreases by having glucose tablets and insulin readily available and ideally a CGM device. As previously stated, exercise in those with T1DM makes glycemic control more challenging, but since I enjoy it so much, I prefer to deal with the glucose fluctuations rather than to forgo the exercise. Hope that helps.
LikeLiked by 1 person
The weightlifting meet started at 11 am and I finished about 12:30 pm on 3/26/2017. Since my body weight is a few kilos below my weight class (77 kg), I decided to eat breakfast prior to weigh-in at 9 am. My fasting blood glucose (BG) was 141 mg/dl so I took 6.5 IU Humalog breakfast bolus.
* Is your fasting often 141mg? It’s high. When I changed from Lantus to Levemir (2 injections a day) my fasting BGs improved.
After the Humalog had finished working 2.5 hrs after the dose at 9:30 am, BG was 123 mg/dl.
* So you were 123mg at 12pm and 184 at 12:30pm. Yes, that’s stress all right 😦
After my lifts were finished my BG was 184 mg/dl which is not unusual (stress hormones are increased by intense exercise). I took a 2 IU Humalog correction dose and 2.5 hours later, my BG was 108 mg/dl.
* Pity about the stress hormones. Would a metformin a couple of hours before lifting allay the rise…?
Prior to dinner (at 6:30 pm) my BG was 61 mg/dl and I took a smaller than usual Humalog dose of 2 IU with dinner along with 28 IU of Lantus. Two hours later, I was not not behaving normally (laughing for no particular reason) and was sweating and my BG was LO on my Freedom Freestyle meter which means <20 mg/dl (That is the lowest I have ever recorded and were I not on a ketogenic diet probably would have had a seizure or worse). It took a total of 6 glucose tablets (24 grams of dextrose, also a first, usually I take 1-2 tabs for a hypo) to bring it up to 75 mg/dl.
* Wow! You really need a CGM. My Freestyle Libre gives an arrow to show if BG is rising, falling or stable. I haven’t had any LOs since getting it (a year ago) … the lowest I’ve gone is 45mg. But apparently the Medtronic device has better graphics and real-time tracking for hypo avoidance.
I gave you these details because you asked. However, the BG response to exercise is quite variable and not predictable unfortunately. My BG has dropped during weightlifting and has also remained unchanged. Seems the determining factor is the intensity of the exercise and the basal dose of insulin (Lantus) at the time.
* So, it's not as unpredictable as all that as you know the determining factors. Could you add to your tables a place where you note the onboard basal insulin and the strenuousness of the exercise? For example the weightlifting should (if I have understood an article I read correctly) result in greater insulin sensitivity over a number of hours after exercise, while aerobic exercise will make you low as you exercise or just after. After a few entries you might be able to analyse the data to find a pattern.
My suggestion is to be prepared for both increases and decreases by having glucose tablets and insulin readily available and ideally a CGM device.
* Yes, the CGM is a Godsend. But I hate adding glucose to an already overweight (but getting thinner) body and converting it to fat right away. Without weights, I now have BGs between 80 and 110 (my targets, not my doctor’s) + weight loss.
* When I wrote to you, I was thinking of reducing cardio in favour of weights etc. in order to reduce the hypos of cardio and to spread the BG descent over time (and increase insulin sensitivity).
As previously stated, exercise in those with T1DM makes glycemic control more challenging, but since I enjoy it so much, I prefer to deal with the glucose fluctuations rather than to forgo the exercise. Hope that helps.
* That helps a lot. Thanks. PS I don’t love exercise at all – I do it to only stay well.
LikeLike
* So you were 123mg at 12pm and 184 at 12:30pm. Yes, that’s stress all right 😦
No, at 9:30 am, BG was 123 mg/dl, and 184 at 12:30pm.
* Pity about the stress hormones. Would a metformin a couple of hours before lifting allay the rise…?
I don’t think so, remember the stress hormones are normal for the purpose of increasing nutrients (glucose and fatty acids) to exercising muscles. This occurs in non-diabetics as well, i.e. no reason to prevent this from occurring. Those with T1DM just have to manually correct it afterwards with insulin.
* Wow! You really need a CGM.
I know.
* So, it’s not as unpredictable as all that as you know the determining factors. Could you add to your tables a place where you note the onboard basal insulin and the strenuousness of the exercise? For example the weightlifting should (if I have understood an article I read correctly) result in greater insulin sensitivity over a number of hours after exercise, while aerobic exercise will make you low as you exercise or just after. After a few entries you might be able to analyse the data to find a pattern.
I did that and could not find a correlation. Remember what seems stressful or difficult to me is not necessarily the same as how my body and its hormonal response perceive it.
* Yes, the CGM is a Godsend. But I hate adding glucose to an already overweight (but getting thinner) body and converting it to fat right away. Without weights, I now have BGs between 80 and 110 (my targets, not my doctor’s) + weight loss.
I don’t agree. The glucose used to correct hypoglycemia is not converted to fat, rather it remains in the bloodstream and later used as your body requires for multiple purposes. Taking glucose should never be avoided during hypoglycemia unless you have a death wish.
* When I wrote to you, I was thinking of reducing cardio in favour of weights etc. in order to reduce the hypos of cardio and to spread the BG descent over time (and increase insulin sensitivity).
Sounds reasonable, just remember the results of doing so, in my opinion, is not necessarily predictable. So be ready for anything.
* That helps a lot. Thanks. PS I don’t love exercise at all – I do it to only stay well.
You’re welcome.
LikeLike
“The glucose used to correct hypoglycemia is not converted to fat, rather it remains in the bloodstream and later used as your body requires for multiple purposes.”
Ah OK, I see, however, just having that glucose in the bloodstream kicks me out of ketosis, right ? (And yes, I agree that hypos must always be treated with glucose immediately – no death wishes here) 🙂
LikeLike
Glad we agree on treating hypos with glucose. Regarding the state of ketosis, I seriously doubt 4-8 grams of dextrose would reverse the benefits of ketosis for T1DM. The blood beta-hydroxybutyrate (BHB) concentration might fall during hypoglycemia by several factors. One: the direct inhibition of HMG CoA synthase, the rate limiting enzyme in ketone body synthesis, by insulin. Two: the inhibition of fatty acid release from fat cells by insulin as fatty acids are the substrate for ketone body synthesis. Three: the consumption of ketone bodies by the brain and other organs during hypoglycemia. However, this reduction in BHB would be temporary and in fact later reversed by treating the hypoglycemia with dextrose as it would resolve the relative insulin excess.
Regarding body fat loss in T1DM, this is most easily accomplished on a ketogenic diet since the diet suppresses hunger allowing a reduction in caloric intake. Since dietary protein and carbs are relatively fixed on the ketogenic diet, dietary fat is the macronutrient that should be modestly reduced to shed excess body weight. This is easy to accomplish by reducing any added fats like dairy (butter, cheese, cream), olive and coconut oil and if needed, leaner cuts of meat. This will likely require a reduction in insulin dose as body weight declines, but insulin doses are always adjusted anyway to achieve one’s selected target blood glucose.
LikeLiked by 1 person
Thanks a lot for that priceless info. If you ever decide to practice in Belgium, I’ll be your 1st patient. 🙂
LikeLike
Thanks, much appreciated.
LikeLike
Hi, My question is in regard to what your mentioned in your comments. If you had before dinner already low BG of 61 mg/dl what was the purpose of taking the Humalog? My understanding is that Humalog is used only to correct the BG if it is high before the meal. Also I have been told not to inject Lantus at the same time as Humalog because the Humalog interferes. I have noticed that when I injected them together at dinner the blood sugar in the morning was higher than usual, and it happened several times until I gave more time between the Humalog and Lantus. Have you noticed that as well? Thank you!
LikeLike
Hi Svet,
The Humalog before dinner has two purposes. One to cover the protein and carbohydrates in the meal. The dose needed is a guesstimate. Then that dose is reduced by some amount if the pre-dinner BG is low as in the case your referring to or increased in the case of an elevated pre-dinner BG.
There is no problem injecting Lantus at the same time as Humalog. What is true is that they cannot be drawn up into the same syringe to be injected. The two insulins do not interfere with each other after being injected in different locations from different syringes and should have nothing to do with an elevated BG the following morning. The response to Lantus (and Humalog for that matter) varies from day to day. That is one of the problems that those with T1DM face on a daily basis. To me, a recurrently elevated morning BG means the Lantus dose needs to be increased a little bit.
LikeLiked by 1 person
Svet, I should have added to my response that there are times when it is appropriate to not give Humalog for a meal. Coincidently, I am in one of those situations right now. This occurs about once a year when I get more hypoglycemia for unclear reasons and have to reduce both Humalog and Lantus doses. During these times taking even 1 IU of Humalog results in hypoglycemia, so I take no Humalog with the meal (this is usually dinner i.e. after exercise).
LikeLiked by 1 person
Dear Keith, I appreciate your detailed response!
LikeLike
I’m curious as to your thoughts on a type one diabetic named Robby Barbaro He eats an extremely low fat high carbohydrate plant-based diet. He has videos on YouTube and has been on several Podcasts. His blood sugars seem incredibly stable given his extremely high carbohydrate diet. He claims this way of eating keeps his body very insulin sensitive. And he coaches other diabetics to adopt this way of eating. Is it possible that the other end of the spectrum, high carbohydrate low-fat, is another solution to controlling blood sugars?
LikeLike
Thanks for the comment, Will. First, regarding type 1 diabetes. I spent about 15 mins trying to find some information about Robby’s glycemic control and insulin doses, but came up empty. This is one of the reasons I started the blog, so that anyone can see exactly how my insulin doses and blood glucose (BG) values changed before and after the ketogenic diet. Also, I report every BG reading and every dose of insulin, not just short stents of time when things are going well. Not even Dr. Richard Bernstein does that. Bottomline, I can’t really evaluate what Robby is doing with his fruitarian diet. The mechanism by which eating mostly fruit and some other very low fat vegetables results in both improved glycemic control and lower insulin doses as well as improved health is not clear to me.
Second regarding type 2 diabetes, I think it is possible to not develop type 2 diabetes on a real-food higher-carbohydrate diet assuming one does not become overweight and remains physically active. Take the Kitavan’s, for example, who were studied in detail by a group of Swedish researchers. The same diet might improve type 2 diabetes in some percentage of cases if they were able lose their excess body fat and be physically active. The difference between a Western high-carb diet and the Kitavan high-carb diet is a lot more dietary fiber, no sugar, no grains, no alcohol, i.e. no processed food of any kind. So what about a fruitiarian diet for type 2 diabetes? If the diet was devoid of processed food and one ate whole raw fruits and vegetables and they lost their excess body fat, they may see some initial improvement in glycemic control due to an improvement in insulin resistance (primarily from the body fat loss). However, I am not aware of any long-term studies that might confirm that and that other nutritional deficiencies might arise were the diet to be followed for years or what supplements would be needed to try and make it more sustainable. Even though I would not tell anyone, let alone a diabetic, to try a fruitarian diet, I think a short trial of it would quickly answer the question in the short-term as to whether or not it is effective for them. If not, the question is answered, if so, then a closer look at preventing long-term nutritional deficiencies would be required.
LikeLiked by 2 people
Thank you. Robby actually goes beyond showing individual blood glucose measurements. He wears a Dexcom and shows the 24 hour graphs on his You Tube channel. The latest video showed a 24 hour BG graph showing that his BG stayed between 62 and 107 mg/dL while eating 750 g of carbs throughout the day. Despite taking fairly large does of Humalog insulin, roughly seven units for each meal, he bosts high insulin sensitivity. He measures insulin sensitivity as total grams carbs / total insulin. On this particular day, Robby calculated his insulin sensitivty at roughly 19:1.
I think you’re right. If one is relatively insulin sensitive, physically active, and consuming real food there are probably several dietary approaches to staying healthy and lean.
Thanks for your help.
LikeLike
I didn’t find that video, but saw another video . The insulin sensitivity formula is something he made up and I do not think being “sensitive to insulin” by that measure is as important as the total daily insulin dose and glycemic control. Eating mainly carbs from fruit will result in a larger insulin dose compared to a ketogenic diet. Anyway, thanks for your interest in my blog. I will listen to your interview with Christopher Kelly later this evening. I did a podcast with him as well.
LikeLike
Hi Keith – What do you think about dosing fast-acting insulin prior to a weight lifting session? I see you mentioned that you hadn’t done it for fear of hypoglycemia. I haven’t done it myself for the same fear… but I’ve thought that I could possibly enhance my performance by giving it a try for certain types of efforts. My sport is a little different (cycling), but sometimes I’ll do hard efforts that last 5-6 minutes. I find it amazing that my liver can more than double the concentration of glucose in my bloodstream within 2 minutes (say 80mg/dL -> 180mg/dL). My thoughts were that this glycogen is being broken down for a reason, and that as a T1D, my muscles simply can’t use it at the rate they were designed to. If I pre-injected some fast acting insulin, and started a 5 minute sprint about 20-30 minutes post-injection, my muscles could better access the glucose that is very rapidly being dumped by my liver. What is your opinion on that theory? I haven’t gotten the courage to try this yet. A second question on the same theme: Have you seen CGM data from non-diabetics performing intense exercise (either lifting or hard VO2max intervals as I mention)? I’m intensely curious to know if non-diabetics also rise up above the oft cited 140mg/dL ceiling for healthy individuals. If healthy individuals also rise to ~180mg/dL, then perhaps my theory is bunk.
LikeLike
Those are important questions Brian. Blood glucose normally increases with intense exercise under the signal of cortisol, epinephrine, growth hormone, and glucagon, presumably to supply exercising with extra glucose and fatty acids. In persons with T1DM, there is no insulin response once the exercise is finished to restore blood glucose back to normal. It is a common misconception that cells can’t use glucose without insulin being present. That is not true. Glucose transporters are always present in the cell membrane to bring glucose into the cell, muscle cells in this example. Insulin serves to increase the number of glucose transporters in cell membranes so insulin does augment glucose transport. Here is an example of a non-diabetic doing intense cycling whose interstitial glucose on a CGM increases to 180 mg/dl and then returns to normal in about 2 hours.
What I do and my suggestion to you is to take a small dose of rapid-acting insulin after the exercise is finished to correct any significant elevation of blood glucose that you might experience rather than trying to guess what your blood glucose will do in advance and taking insulin based on that guess. I do not think preventing the rise in blood glucose would improve your performance, but I am sure that hypoglycemia would worsen performance or create other adverse circumstances for you to have to deal with. I hope that helps.
LikeLike
Keith – Thanks for your thoughtful reply. I had already seen Chris’ report of going high after intense exercise (and actually, his racing glucose profile seems to match my diabetic one when I run solely on basal during intense efforts). I guess I was curious if there are other people besides this n=1. Maybe I’ll convince some of my nerdy athletic friends to do some sprints and fingersticks! I’ve been doing what you suggest (post-effort injection of 1U Novolog), and that brings it back down quite quickly. Seems Novolog acts more quickly in hot, sweaty skin. I have a question for you about glucose transporters. You say that “It is a common misconception that cells can’t use glucose without insulin being present”. Would you be able to explain that or point me to a resource that explains how muscle cells can use glucose in the absence of insulin? Right after diagnosis, but before my doctor could prescribe insulin, I went on some endurance pace bike rides to see if I could bring my blood glucose down. Instead, blood glucose just kept creeping up (I spent that week hanging out at 300-400mg/dL all day until she got me insulin). This elevated glucose was not the same as doing an intense effort where cortisol, epinephrine, and glucagon cause the liver to dump glycogen. This n=1 observation led me to believe that we need at least some insulin on board for the muscles to utilize glucose.
Slightly off topic, but I noticed you have some experience with endurance (Triathlon), and I was wondering what you think about the following. I do some really long ultra activities (my most recent was the GDMBR where I raced about 20 hours per day for 14 days). During that time, I consumed about 1,000g carb per day and averaged 12U Lantus per day – only occasional 1U corrective bolus after stopping before bed. Blood sugars averaged ~114mg/dL – I’d spike up to 180mg/dL after eating carbs – but return to 80’s within 1hr if I kept riding @ ~70% of max heart rate (i.e. aerobically). The problem with ultra riding is that you need to take rest days. During my rest days, I find that my I:C ratio is a horrible 1:5! While endurance racing (aerobic, steady, 75% of max heart rate), I:C is 1:500+ Trying to follow my slightly higher carb version of the Dr. Bernstein diet is pretty crazy because every day is so different. During a rest week, I’ll be injecting 16U of basal and 12U Novolog to dispose of about 60g daily carb. During really big training days, I find that I need to eat hundreds of grams of carb just to “feed” 12U Lantus and zero Novolog. One possibility (albeit complex) would be to reduce the basal during big training days so I can stay low carb… The other possibility is just to do what I’m doing and consume a lot of carbs to feed the insulin – in other words, make the adjustment on the food end instead of the insulin end. What do you think would be better? What do you think about my really low I:C ratio when resting – do you think it is due to being accustomed to high levels of exercise? I can’t help but wonder what would happen to the I:C ratio if I took a long break from endurance exercise. As a note, both my parents were Type 2 (I’m type 1 for sure (IA-2 and GAD antibodies in very high titer)… but have no way of identifying if I’m also type 2). Thanks again for any thoughts you may have.
LikeLike
Brian, again you bring up several important points.
1. If you can get any non-diabetic friends to measure BG after intense exercise, please report back the results. I have found several papers that show the increase in glucose and the hormones I mentioned in the previous response with intense exercise. Here is one of those papers.
2. As previously mentioned, glucose is transported by facilitated diffusion which does not “require” insulin. The greater the concentration difference of glucose on either side of the cell membrane, the faster the transport of glucose. Insulin can increase the rate of glucose transport by increasing the number of transporters in the cell membrane. This page explains it pretty well.
3. I experienced the same changing I:C ratio while training for triathlons. I attributed the difference to changing insulin sensitivity between exercise days and rest days. It is known that the improved insulin sensitivity due to exercise lasts between 24-72 hours. Mine seemed to last only 24 hours. Thus, I was changing insulin doses daily to compensate. I have tried many different strategies to compensate for this problem, but honestly I can’t say I have mastered this problem. Now with weightlifting, I alternate olympic weightlifting one day with general less-intense bodybuilding type weightlifting the next day. This regularity of schedule makes managing BG a little easier as apposed to doing a 100 mile bike ride followed by 2 days rest, followed by a swim and run day, then 1 day rest, etc. etc. i.e. a much more variable exercise schedule. I also tried what you suggest of changing Lantus doses and even split it into two doses per day for about 3 months. I abandoned that approach for lack of efficacy. I think it doesn’t work because the 12 hour half-life of Lantus means it takes 3 days of a constant new dose to reach a new steady-state. I think keeping the basal insulin constant and taking carbs as needed is the better approach. Besides, your muscles can make good use of those carbs during exercise.
4. If you took a long break from endurance exercise, you would initially have to increase your insulin doses over the week or two at most, then the insulin doses would level off and stabilize. Even though I really enjoy exercise and don’t want to stop, I think my BG would be easier to manage if I didn’t exercise and still remained on the ketogenic diet.
5. Insulin resistance can occur in those with T1DM. Typically, they will be overweight, have elevated triglyceride and low HDL-C levels, elevated hs-CRP levels, and have high insulin requirements. With your lower insulin doses and exercise regimen, I would be surprised if you had any of those markers for insulin resistance.
I hope the above helps.
LikeLiked by 1 person